Tue, Dec 19, 2023
Read in 5 minutes
Allergic rhinitis is the inflammation of the inside of the nose that occurs due to allergens like dust, mould, pollen, insects or even skin flakes. Allergic rhinitis, called hay fever, causes congestion, sneezing, sore throat and itchy nose. A study conducted among children showed that 11.3% of kids as young as 6 or 7 years show signs of allergic rhinitis, but there is no reason to fret, as, with just a few lifestyle changes and proper care, you can easily overcome it. Allergic rhinitis can blunt the sense of smell, and it can also interfere with the other important functions of the nose. When your nasal passages are functioning normally, about five to eight quarts of air pass through them each minute. Your nose has the job of conditioning that air before it reaches the sensitive tissue of your lungs. Your nose adds moisture, but to do that, it must produce large amounts of mucus. It also warms the air, with help from a large network of blood vessels. Finally, the nose traps small particles, keeping them out of the lungs.
What Is Allergic Rhinitis?
An allergen is usually a harmless substance but can cause the release of a natural chemical known as histamine in your body. It is believed that between 10% and 30% of the population worldwide may suffer from allergic rhinitis. This can cause significant morbidity, healthcare costs and, in most cases, loss of productivity.
Allergic rhinitis is generally classified as either:
• Seasonal (also called hay fever)
• Perennial (year-round)
Common Triggers of Allergic Rhinitis
1. Pollen: Pollen from trees, grasses, and weeds can be a significant trigger, leading to seasonal allergic rhinitis (commonly known as hay fever).
2. Dust Mites: These microscopic creatures are commonly found in bedding, pillows, and upholstered furniture. Their waste particles and body fragments can trigger allergic reactions.
3. Pet Dander: Skin flakes, urine, and saliva from pets, such as cats and dogs, can cause allergic rhinitis in susceptible individuals.
4. Mold Spores: Mold grows in damp environments, and the spores released into the air can trigger allergic reactions. Indoor areas like bathrooms, basements, and kitchens are common places for mold growth.
5. Air Pollution: Environmental pollutants, such as smoke, car exhaust, and industrial emissions, can irritate the nasal passages and worsen symptoms in individuals with allergic rhinitis.
6. Certain Foods: In some cases, certain foods can cross-react with allergens and trigger allergic rhinitis symptoms. This phenomenon is known as oral allergy syndrome.
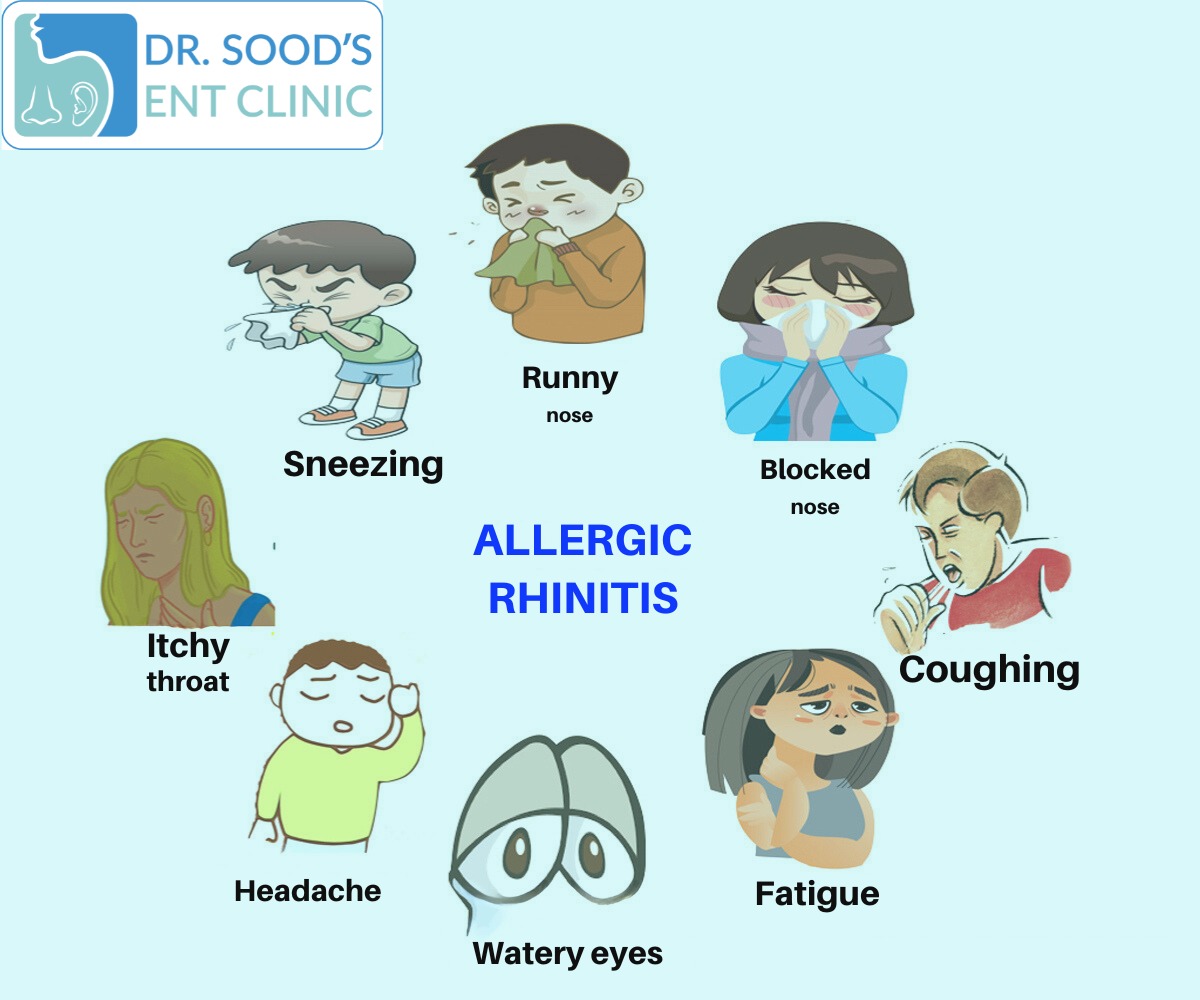
Symptoms
- Runny or Stuffy Nose
- Sinus Pressure
- Sneezing
- Itchy Eyes
- Postnasal Drip
Treatments
Allergen Avoidance:
Identify and avoid allergens that trigger your symptoms. This may involve minimizing exposure to pollen, dust mites, pet dander, mold, and other environmental triggers. Use air purifiers with HEPA filters to reduce airborne allergens indoors. Keep windows closed during high pollen seasons.
Nasal Irrigation:
Nasal irrigation with saline solution can help clear nasal passages and reduce the presence of allergens. saline nasal sprays are commonly used for this purpose.
Antihistamines:
Over-the-counter or prescription antihistamines can help relieve symptoms such as sneezing, itching, and runny nose. Examples include cetirizine, loratadine, and fexofenadine.
Immunotherapy (Allergy Shots):
For individuals with severe and persistent allergic rhinitis, allergen immunotherapy may be recommended. This involves gradually exposing the individual to increasing amounts of the allergen to build tolerance.
Prescription Eye Drops:
If allergic rhinitis includes eye symptoms (allergic conjunctivitis), prescription eye drops containing antihistamines or mast cell stabilizers may be recommended.
Medication Many treatments are available. Here’s a quick summary of the major types.
Antihistamine tablets will help most patients. For the majority of people, one of the less sedating preparations will be best. Many are available over-the-counter,
Nasal steroid sprays budesonide , fluticasone , and triamcinolone which are available without prescription.
Antihistamine nasal sprays are an alternative to oral antihistamines. Azelastine (Astelin)
Leukotriene blockers, such as the oral prescription drug montelukast (
Decongestants are available without prescription as tablets (pseudoephedrine, phenylephrine) or nasal sprays (phenylephrine, oxymetazoline) and can relieve nasal congestion but have little effect on other allergic rhinitis symptoms.
Other medications include an anticholinergic nasal spray called ipratropium (Atrovent), which is effective only for runny noses and various anti-allergic eye drops can be used to treat eye symptoms.
Immunotherapy, or “allergy shots,” can help achieve long-term control of allergic rhinitis. The regimen usually involves skin testing to identify the responsible allergens followed by weekly injections of gradually increasing doses of the allergen, and then maintenance injections every two to six weeks for several years. Most doctors reserve immunotherapy for patients who do not respond well to medication.
Prevention
Nasal Irrigation:
Regular nasal irrigation with saline solution can help flush out allergens and reduce nasal congestion.
Personal Hygiene:
Wash your hands frequently to prevent the transfer of allergens to your face. Shower and change clothes after spending time outdoors during high pollen seasons.
Healthy Diet:
Adopt a healthy diet rich in fruits, vegetables, and whole grains. Some studies suggest that certain nutrients may have a protective effect against allergic conditions.
Regular Exercise:
Engage in regular physical activity to support overall health. Exercise can help improve lung function and may have positive effects on allergy symptoms.
Consult an Allergist:
If you suspect you have allergies, consider consulting an allergist for proper testing and diagnosis. Knowing your specific triggers can help you implement targeted preventive measures.
